Many rooms in hospitals require special design considerations due to intensified infection concerns, high air change rates, special equipment, unique procedures, high internal loads, and the presence of immunocompromised patients. But in no other healthcare space does the design of the HVAC system take on more importance than in an operating room (O.R.), where its purpose is to minimize infection, contribute to an environment of patient care, and maintain staff comfort.
Hospital operating rooms are notoriously plagued with environmental control problems revolving around the inability to maintain temperature and relative humidity conditions that comply with various healthcare codes and standards while satisfying the comfort demands of surgeons and staff. This article will provide an understanding of the underlying causes for some of the most predominant of these issues, while giving guidance on how to best cope with them. Unfortunately, many hospital facility professionals have resigned themselves to the idea that these problems cannot be resolved, which is often far from the truth.
COMPLAINT: “Why do surgeons want the operating room cooled to such low temperatures, many times demanding 60°F (15.6°C) or colder?“
CAUSE: Many surgeons, particularly those performing orthopedic (or other highly invasive procedures), are heavily gowned in multiple layers of outer garment, while wearing face and head protection encapsulating their entire body. This protects both staff and the patient from the transfer of bodily fluids and potential bloodborne or airborne contamination. These surgeons are using an array of surgical instruments including hammers, chisels, and saws, while working diligently under intense lighting in what is a highly physical and mentally taxing environment.
Surgeons quicky begin to perspire (sweat) under these circumstances, becoming physically hot and wet, which leads to immediate distraction and discomfort. Their first inkling is a feeling that they’re too hot. So they demand relief through the lowering of the room’s temperature setpoint in hopes of establishing a more comfortable environment.
When humans feel too warm, they seek cooler surroundings. Any relief we may experience indoors comes, in large part, from achieving the proper combination of temperature and relative humidity. Relative humidity plays a major role in our body’s ability to cool (and remain cool) as it impacts the evaporation of perspiration from our skin. Lower relative humidity assists in the evaporation of moisture and is the underlying principle behind evaporative cooling.
We are constantly perspiring, and the evaporation of this moisture absorbs approximately 1,060 BTU/hr of internal body heat for every one pound of perspiration removed. To effectively achieve this, increasing our skin’s exposed surface area and/or lowering relative humidity may be necessary.
Surgeons who are heavily gowned have very little skin exposed to the ambient air, so unless the relative humidity (and associated air moisture content) in the environment they occupy is low enough to help assist in evaporating (wicking) this moisture through multiple layers of clothing and into the surrounding air, they may receive little if any relief in this regard. Surgeons in these situations have compared what they are experiencing to that of being wrapped in a sheet of plastic. They may be sweating profusely, experiencing extreme discomfort, and losing focus, all of which may seriously impact their performance and the patient’s outcome.
CURE:
The O.R. must be controlled to that combination of temperature and relative humidity which can achieve thermal comfort while also accounting for the evaporative cooling effect mentioned above. In orthopedic surgical suites the combination of conditions that best satisfy surgical staff in these situations has been found to be 60°F (15.5°C) at 40% relative humidity.
##########
COMPLAINT: “When I lower the operating room space temperature (at the request of the surgeon) the relative humidity goes up!”
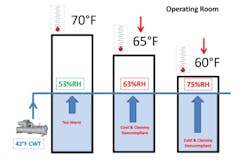
CAUSE: Most hospital central utility plants produce and provide a chilled water temperature (CWT) of 42°F (5.6°C) which is pumped to an HVAC system cooling coil tasked with cooling and dehumidifying supply air for distribution throughout the facility. While this CWT may be cold enough to produce satisfactory (sensible) temperatures, it is usually not cold enough to properly dehumidify the air in order to achieve the lower relative humidity conditions required in the O.R. space.
You can see what happens in Figure 1.1 when the space thermostat setpoint is lowered from 70°F (21.1°C) down to 60°F (15.6°C), upon the surgeon’s request for a more comfortable environment.
While 42°F (5.6°C) CWT can easily provide air cold enough to maintain a 60°F (15.5°C) space temperature, the cooling coil’s surface can only be chilled to approximately 45°F (7.2°C). This drastically limits the ability of the coil to condense enough moisture from the air to achieve a corresponding low dew-point temperature, and results in an increase in O.R. relative humidity whenever the space temperature is lowered. With higher relative humidity, less evaporation of perspiration is occurring, and staff continue to perspire underneath their gowning. Sweat is also being absorbed into their clothing, making it wet, resulting in distracted and disgruntled surgeons and staff. At this point, O.R. relative humidity may be well outside of compliance with healthcare codes and standards which mandate a maximum of 60% RH be maintained.
CURE:
1. Raising O.R. space temperature (with reheat) may lower the relative humidity, but if the resulting temperature becomes too warm, surgeon comfort may still be sacrificed;
2. Adjust the thermostat’s cooling setpoint downward to that temperature which coincides with a space relative humidity that remains within compliance to applicable healthcare codes and standards for O.R. environments. Understand that a colder space temperature, along with a higher relative humidity, may be less comfortable for staff than a higher temperature coinciding with a lower relative humidity. The evaporation of perspiration from the surgeon’s skin and gowning is paramount to their satisfaction;
3. Lowering the CWT cold enough to properly dehumidify the air may be deemed necessary for O.R. staff comfort and productivity. This solution is very limited in its practicality if chillers were not originally sized for this change, as it may negatively impact the performance, efficiency, and capacity of the entire HVAC chilled water system;
4. Facilities dealing with consistently high space relative humidity, or excursions in humidity that create negative consequences in the O.R., should be analyzed for HVAC equipment and controls upgrades specifically designed to handle the stringent dehumidification demands of critical care environments.
##########
COMPLAINT: “At times, it ‘rains’ in the operating room, with water dripping from surfaces.”
CAUSE: “Raining” in the O.R. (as it is often termed) is the occurrence of liquid condensation on cold surfaces. This condensate can accumulate and drip into the space, onto sterile medical devices and instruments, onto surgical staff, or perhaps into the surgical opening of a patient.
Moisture in the air can be condensed on any surface which has been chilled below its dew-point temperature, much in the same way high humidity in the air is condensed onto a cold cooling coil, or onto a cold can of beer on a hot, humid summer day. This phenomenon occurs in the O.R. when surfaces have been chilled below the humidity equilibrium (dew-point) of the surrounding air. This chilling effect is usually a direct result of a temperature setpoint which has been lowered at the request of surgeons and staff seeking improved comfort.
When this condensation occurs during surgery, it places the procedure at considerable risk. Water harbors microbial contamination, some of which may be harmful or deadly if a patient is exposed and cross-contamination occurs. It is a concern regarding the occurrence of surgical site infections (SSIs), hospital acquired infections (HAIs), and jeopardizes any healthcare code compliance as the O.R. is usually well above 60% RH at this point.
CURE:
1. In these situations, raising O.R. temperature (with reheat) may help warm chilled surfaces above the air’s dew-point temperature, while also lowering the space relative humidity to begin mitigating condensation, but if the situation has already occurred, it’s an effort employed too late. In addition, if the resulting space temperature becomes too warm, surgeon comfort may be sacrificed.
2. Monitor the combination of O.R. temperature and relative humidity to determine its dew-point, and ensure it always remains well below the temperature of any chilled surfaces in this space. Overhead HVAC supply air registers are usually going to be the coldest object, are constructed from non-porous material which easily drips water, and therefore may be the first point of concern with moisture condensation. The grille’s surface temperature will approximate that of the HVAC system supply air. If the leaving air temperature from the grille is 55°F (12.7°C), then the space dew-point temperature should be maintained at least 4°F (2.2°C) lower, so no higher than 51°F (10.5°C). Note that under these conditions and with lower space temperatures, the O.R. may be above 70% RH. So much lower supply air dew-point temperatures are usually required. This is not achievable with chilled water temperatures of 42°F (5.6°C).
3. Measure and control O.R. conditions to maintain relative humidity below the maximum mandated in applicable healthcare codes and standards for the facility. This usually calls for an upper limit of 60% RH.
4. As relative humidity in the space rises above code mandated maximums, your choice(s) in reducing it include lowering the chilled water temperature to HVAC system cooling coils, applying terminal reheat to warm the air, or both. This should be an automated function through the controls system which safeguards the space. Note that if the resulting space temperature becomes too warm, surgeon comfort may be sacrificed.
5. Facilities dealing with consistently high space relative humidity, or excursions in humidity that create negative consequences in the O.R., should be analyzed for HVAC equipment and controls upgrades specifically designed to handle the stringent dehumidification demands of critical care environments.
#########
COMPLAINT: “On days when outdoor relative humidity is low, why does the humidity in the hospital facility increase when more ventilation air is introduced?”
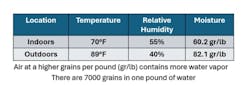
CAUSE: Relative humidity alone has no significance in determining the actual amount of water vapor (moisture) contained in a particular sample of air. It is the amount of moisture in the air we are concerned with when designing air-conditioning and dehumidification systems that can properly remove it. As its name implies, relative humidity is a “relative” term, and must be considered in combination with temperature to assess the amount of water vapor an air sample contains by weight, or in grains per pound.
Don’t be fooled into thinking that just because an air sample has a low relative humidity, it is always “drier” than that which is at a higher relative humidity. This is often a false premise, leading to facility operators mistakenly bringing in “moister” outdoor ventilation air in a misguided attempt to save energy on the HVAC system’s operation.
Figure 1.2 shows two ambient air conditions: one is indoors at a higher relative humidity, while the other is outdoors at a lower relative humidity. As can be seen, the outdoor air contains much more moisture in this case. Limiting the amount of this air brought into the HVAC system, while always maintaining healthcare code required ventilation rates, would be less taxing on the HVAC equipment.
CURE:
1. Always maintain healthcare code required outdoor ventilation rates. These should be measured and monitored to ensure compliance.
2. Don’t arbitrarily bring in excess outdoor ventilation air (above code minimum) without first understanding the psychrometric properties of both the indoor and outdoor air conditions. If you increase ventilation air, have a sound reason for doing so. If you bring in additional outdoor air, understand that it may negatively impact space pressurization balances unless additional exhaust is provided.
3. Facilities dealing with consistently high space relative humidity, or excursions in humidity that create negative consequences in the O.R., should be analyzed for HVAC equipment and control upgrades specifically designed to handle the stringent dehumidification demands of critical care environments.
SUMMARY:
Many times, surgeons seeking relief from heat stress will demand “colder” O.R. temperatures, when what they really need is “drier” space air to assist in evaporating perspiration from their skin and garments.
Battling the environment in hospital O.R.s doesn’t have to be a fight that is always lost. There are resolutions to help hospital engineers and facility managers deal with the consistent problem of high relative humidity in these spaces. While some are a temporary, “band-aid” style approach, permanent solutions are available including solid desiccant dehumidification. It is a proven HVAC technology that can ensure compliance with healthcare codes and standards while catering to the demands of surgeons and staff seeking a more comfortable and productive environment.
REFERENCES
1. ASHRAE HVAC Design Manual for Hospitals and Clinics, Second Edition, 2013.
2. ANSI/ASHRAE/ASHE Standard170-2021 Ventilation of Health Care Facilities.
3. FGI Guidelines for Design and Construction of Hospitals and Outpatient Facilities, 2014 Edition.
4. ASHRAE Journal, Conditioning for the Environment of Critical Care; Hospital Operating Rooms, October 2019.
5. ASHRAE Journal, Avoiding Wet & Moldy AHUs in Critical Care Facilities, November 2023.
6. ASHRAE, Understanding Psychrometrics, Third Edition, 2013.
7. Journal of Industrial Textiles, Development of Breathable and Liquid/Wet Bacterial Penetration Barrier Composite Laminated Fabrics for Surgical Gown Applications, 2023.
ABOUT THE AUTHOR
David N. Schurk DES, CEM, LEED-AP, CDSM, CWEP, SFP, CIAQM, is the "Dehumidification Jedi" at Innovative Air Technologies in Covington, GA. He is an ASHRAE Distinguished Lecturer and has over 40-years of experience in the design and analysis of heating, ventilating, and air-conditioning systems for a variety of market sectors, with a special focus on aerospace and healthcare facilities. He can be reached at 920-530-7677 or [email protected]
##########