By DAVID SCHURK, DES, CEM, LEED-AP, CDSM, CWEP, SFP, CIAQM, CHC, Global Plasma Solutions
There is much we have yet to learn about the virus SARS-CoV-2 that causes the disease COVID-19. We do not know, for example, when an infected individual breathes, talks, coughs, or sneezes into the air how many actual virons are encapsulated in the respiratory droplets that are emitted into the surrounding environment (viral sheading). We also do not know how may virons it takes to cause an infection when a susceptible host in that same environment inhales these respiratory droplets (quantum of infection). While these are questions that may take considerable time to answer, it is surprising how much we have learned in a relatively brief period, about how the virus is (and perhaps is not) being transmitted indoors.
We do know it can be spread via airborne transmission between individuals within built environments. Guidance has been disseminated by several agencies including the Centers for Disease and Control (CDC), the World Health Organization (WHO), the American Society of Heating, Refrigeration and Air Conditioning Engineers (ASHRAE) and others to help us reduce this risk. Valuable information has recently been updated and revised, culminated here into what is most currently available and shared in the paragraphs that follow.
In 2019 (before SARS-CoV-2), a major article was published in the American Journal of Infection Control entitled “Particle Control Reduces Fine and Ultrafine Particles Greater than HEPA Filtration in Live Operating Rooms and Kills Biological Warfare Surrogate” (1), authored by experts in the field of medicine, aerosol science, filtration, and engineering. The document states “The majority of airborne pathogens fall into the fine-particle or ultrafine-particle ranges. It is a common misconception that these small particles are effectively cleared from a space (such as an operating room) via HEPA filtration.”
It goes on to tell us “Unfortunately, most very small particles and pathogens are of insufficient mass to be controlled by bulk airflow and can remain suspended for days or even weeks. Significant fractions of these suspended particles and pathogens cannot be effectively transported to or removed by conventional air filters.”
The authors acknowledged that controlling indoor air quality and the airborne transmission of infectious agents is critical, and that the most hazardous particles and pathogens are not easily eliminated by traditionally passive air cleaning technologies. They concluded that air filters (even HEPA) are only effective on those particles and pathogens that can reach the filter, not those that remain suspended in space. To summarize, although an air filter can be rated as highly efficient, it may not be all that effective in actual use.
In July of 2020, Holt Architects and M/E Engineering combined efforts to perform a computational fluid dynamics (CFD) simulation of Holts workspace, showing how infected droplets might move through their studio office. A person coughing three times in a 10-minute period was shown to produce a cloud of infective aerosols that could be carried more than 50-feet across the space. In conclusion to the simulation, Steven W. Hugo, AIA, and a principal at Holt stated, “Notice that the cloud of virus never reached the mechanical system where filters could be effective.” Video available at https://www.youtube.com/watch?v=3I3G4HN2MEs
Then, in the November 2020 ASHRAE Journal, an “Industry News” interview was published which talked about the ASHRAE Epidemic Task Force and its work in keeping up with the latest information on the virus (2). With a goal to provide guidance on reducing airborne exposure, it was noted that emerging research has not provided evidence of the transmission of SARS-CoV-2 virus through HVAC systems, although within a space, air motion caused by HVAC system components, as well as fans, can be a factor.
In January 2021, ASHRAE Journal printed a peer-reviewed article titled “Preparing HVAC Systems Before Reoccupying a Building” (3) which discussed WHO and CDC recommendations, along with ASHRAE Epidemic Task Force Comprehensive Building Readiness guidance for preparing HVAC systems for buildings reopening after COVID-19 closures. The authors noted that “The growing science around far-afield aerosol transmission essentially negates the need for in-duct or air system control technologies such as UV lights. While these products and services may serve a useful function, in most applications, they may not meet the specific need that is called for in mitigating the hazards of SARS-CoV-2”.
The authors went on to conclude that, “Of course, specialized applications may exist where added levels of in-space or in-room protection may be useful, most notable in healthcare and long-term of senior care facilities.”
On March 23, 2021, the Centers for Disease Control and Prevention (CDC) released updated guidance on virus transmission which appeared on its website and addressed the question, can COVID-19 be transmitted through HVAC (ventilation) systems? It stated:
“The risk of spreading SARS-CoV-2, the virus that causes COVID-19, through ventilation systems is not clear at this time. Viral RNA has reportedly been found on return air grilles, in return air ducts, and on heating, ventilation, and air-conditioning (HVAC) filters, but detecting viral RNA alone does not imply that the virus was capable of transmitting disease. One research group reported that the use of a new air-sampling method allowed them to find viable viral particles within a COVID-19 patient’s hospital room with good ventilation, filtration and ultraviolet (UV) disinfection (at distances as far as 16 feet from the patient). However, the concentration of viable virus detected was believed to be too low to cause disease transmission. There may be some implications for HVAC systems associated with these findings, but it is too early to conclude that with certainty.”
CDC concluded: “While airflows within a particular space may help spread disease among people in that space, there is no definitive evidence to date that viable virus has been transmitted through an HVAC system to result in disease transmission to people in other spaces served by the same system.”
Proper ventilation and filtration are pillars of a well-designed HVAC system and paramount to creating safe and productive indoor environments, but this latest information on how SARS-CoV-2 may (or may not) be transmitted indoors could be an indication that traditionally mounted HVAC system air-cleaning devices might not be as effective in helping reduce an occupant’s exposure to indoor airborne contaminants as desired. The virus may be staying in the space as (aerosolized) droplet nuclei, suspended in the breathing zone indefinitely, possibly remaining infectious for up to several hours. Consideration of treating the contaminants of concern (regardless of what they are) in the space itself may be prudent when implementing an effective strategy to create synergy between indoor social distancing measures (temperature scanning, masks, physical separation, etc.) and an HVAC system that adds an additional layer of occupant protection.
Easily understood is the simple concept that if the pollutants in the space air are removed, they may then no longer be a health risk to people breathing that air. This should be a major accomplishment for all building air cleaning systems moving forward. The question now becomes what can we do to help achieve successful results in the most cost-effective way?
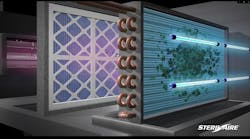
Advanced IAQ technologies should be considered and applied as a “bundled” approach, combined with traditional ventilation and filtration to help enhance overall air cleaning efficiency and effectiveness. They can be included in most new or existing HVAC systems, and many can be applied directly at the space level itself, where contaminant remediation may prove most effective.
The specific technology employed (and how it is applied) should be matched to treat the contaminants of concern when considering what they are, where they are being generated, and how they may be most effectively mitigated. This may prove paramount to improving results when striving for safer, healthier, and cleaner indoor environments for the occupants residing within buildings and structures of all types, everywhere.
References
(1) Mark H. Ereth MD, Donald H. Hess MSME, Abigail Driscoll BS, Mark Hernandez PhD, Frank Stamatatos BEE, Particle Control Reduces Fine and Ultrafine Particles Greater than HEPA Filtration in Live Operating Rooms and Kills Biologic Warfare Surrogate, American Journal of Infection Control, 2019;
(2) ETF Chair: Limited Virus Knowledge is Key Challenge, ASHRAE Journal, November 2020;
(3) John McCarthy, SC.D., C.I.H., Member ASHRAE, Kevin Coghlan, Preparing HVAC Systems Before Reoccupying A Building, ASHRAE Journal, January 2021.
##########
About the author
David Schurk is Director of Healthcare Vertical Markets for Global Plasma Solutions, Charlotte, NC. An ASHRAE Distinguished Lecturer, he is a Licensed Designer of Engineering Systems with over 40-years of experience in the design and analysis of HVAC and air cleaning systems for a variety of market sectors. His special focus is on aerospace and healthcare facilities.