Pressure Management in Health-Care Facilities
Why is air-pressure important to a health-care facility? Health-care facilities are environments in which numerous infectious diseases, some of which are transported by air, must be controlled because of their proximity to patients, many of whom have suppressed immune systems because of their ages or ailments. Another concern is the diseases' proximity to health-care workers, who often unwittingly are exposed to patients who have yet to be diagnosed.
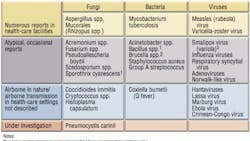
Facility managers, along with safety professionals, are responsible for managing the risks of these hazards. They must establish safe environments for patient care and other everyday work. Mechanical ventilation is used to manipulate pressure differences among various spaces. By creating a differential pressure between two spaces, airflow direction and intensity can be influenced. Examples of microbes that can be spread by air pressure are listed in Table 1.
This article will discuss the concept of pressure control for managing infectious diseases.
Basics
Pressure is the exertion of force on an object. Air pressure can be dynamic, such as wind on a sail, or static, such as air in a balloon. Pressure is defined as force exerted per unit area (i.e., pounds per square inch).
Previously, building pressure management was related to smoke control during fire conditions. Today, in addition to fire management, pressure is utilized to control the indoor environment by containing or excluding contaminants. Hospital pressure management has focused on managing infectious diseases. Since 1947, the United States has relied on building codes to guide hospital pressure relationships. This began with the Hill-Burton Act and has been adopted and revised by the American Institute Architects (AIA), the Uniform Building Code, and the National Fire Protection Association.
The desire to control airflow has been associated with the desire to control airborne infectious diseases. A comprehensive number of diseases spread through the air are listed in the Centers for Disease Control's (CDC's) Environmental Infection Control (EIC) guidelines (Table 1). Before 2001, the AIA guidelines listed air as flowing "in" or "out" of a specific area for pressure (airflow) control. Since 2001, the AIA and CDC have listed a differential pressure of 0.01 in. water column (2.5 Pascals) as the design criteria for airborne-infection-isolation (AII) and protective-environment (PE) rooms (negative pressure for AII rooms and positive pressure for PE rooms). What does such a pressure designation mean? Why should air pressure be managed?
Obviously, air movement should be controlled for fire and smoke management. At the same time, it is important to control infectious agents that could be transmitted via airborne droplet nuclei. By comparison to other routes of infection, few diseases are spread through the air. However, many individuals indulge in the concept that diseases of the future will be transmitted through the air. While the potential is there, the vast majority of past disease dissemination does not indicate airborne transmission (although it is enhanced by overcrowding). Regardless of the probability of airborne transmission, people still must be prepared to control airborne-transmitted infectious diseases. How should mankind prepare and ensure safety in the current environment of hospital care?
During construction, fire codes are "boss codes." The rules associated with these life and safety considerations must be coordinated with other aerosol-management needs. Certainly, people can recognize that because extreme methods of containing smoke can be developed, less-extreme containment for airborne infectious diseases can be developed with the same systems. Hospital fires start less often than in the past. Those that do occur have lower fatality rates because of excellent fire-code considerations when building and managing health-care facilities. While emphasis still is focused on life-safety concerns, that focus is changing to include health-care-acquired infections, even infections spread through the air.
Infectious-disease management is an essential function of a medical facility. The majority of disease is spread by direct or close contact with infectious-disease patients. Relatively common airborne-spread bacteria, such as Mycobacterium tuberculosis or the fungus Aspergillus fumigatus, need to be controlled for a safe environment and the care of patients and employees.
Airborne-infection isolation (AII) is used for diseases recognized to be spread to patients through the air. AII rooms have ventilation parameters for containment of airborne droplet nuclei (Figure 1).
Compare that with a protective-environment (PE) room used to protect patients compromised by surgery, disease, and treatment from opportunistic pathogens (Figure 2).
AII-room engineering features include:
- Negative pressure (greater exhaust volume than supply-air volume).
- A pressure differential of 2.5 Pascals (0.01 in. wg).
- An airflow-volume differential greater than 125 cfm exhaust volume vs. supply-air volume.
- Sealed rooms with an approximately 0.5-sq-ft leakage area per room.
- A clean-to-dirty airflow.
- Monitoring airflow.
- More than 12 air changes per hour (ACH) for new or renovated rooms and six ACH for existing rooms.
- Exhaust flows to the outside or through high-efficiency-particulate-air (HEPA) filters, if air is recirculated.
AII rooms are designed to be depressurized relative to corridors. In other words, air flows from the corridor and adjacent spaces into the AII room. Possible uses include bronchoscopy, autopsy, and certain emergency rooms (Figure 1).
PE-room engineering features include:
- Positive pressure (greater supply-air volume than exhaust volume).
- A pressure differential of 2.5 to 8 Pascals (0.01 to 0.03 in. wg), ideal at 8 Pascals.
- An airflow-volume differential greater than 125 cfm supply-air volume vs. exhaust volume.
- Sealed rooms with an approximately 0.5-sq-ft leakage area per room.
- A clean-to-dirty airflow.
- Monitoring airflow.
- More than 12 ACH for new or renovated rooms and six ACH for existing rooms.
- Return air, if it is refiltered.
PE rooms are designed to be pressurized relative to the corridor. In other words, air flows from the PE room to the corridor. These rooms require ventilation control using room air exchanges for dilution ventilation. This volumetric displacement of air reduces the probability a patient will be exposed to infectious particles. Hospital filtration removes outdoor particles brought in by air-handling systems. If previously conditioned air is recirculated for economization, it is first passed through a filter to remove infectious particles. Pressure controls airflow movement in a building. When people have a reasonable understanding of air volume into and out of a building, they may have control of areas requiring airflow regulation. Possible uses include immunocompromised patient rooms (e.g., solid-organ-transplant procedure rooms) and orthopedic operating rooms (Figure 2).
Airborne-infectious environments and protective environments best exemplify the need for ventilation control. However, construction projects are unique in health care because, often, construction occurs in an occupied building with compromised patients. Ventilation management is necessary during hospital construction to prevent exposure to hazardous airborne microbes (Table 2).
Hospital sustainability comes through the recognition of hazards and the provision of appropriate ventilation with preventive maintenance to ensure proper safety for patients, staff, and visitors. Pressure provides a controlling parameter through fluid control of particles inside a building. Some sources of indoor particles, such as asbestos or aspergillus spores, could be hazardous. Chemicals also follow airflow and commonly are controlled in laboratories with chemical hoods.
Environmental Monitoring
Air particles are common in air both inside and outside of buildings. The presence of airborne particles may be an indicator of air quality if the particles can be identified by kind or concentration. Exposure to minerals, such as asbestos, is a known hazard with regulated practice for control. Infectious or allergenic particles, such as mold spores, are transmitted through the air. Likewise, transmission of tuberculosis is via airborne droplet nuclei originating from an infected person. Management of such aerosols utilizes engineering controls in a ventilation system to direct airborne particles to an exhaust or to dilute a particle to limit the probability of someone breathing it.
Air exchanges provide dilution ventilation to lessen that probability. With increased air exchanges, comfort must be considered. Providing airflow into a breathing zone may create a draft for a sick patient. Therefore, room design should offset a supply diffuser to minimize that draft. Particle control first must provide for source management because of particle generation from common activities, such as cleaning. Such activities can be monitored with a particle counter, but it is difficult to distinguish an aerosol from a cleaning agent or sneeze.
Pressure is a controlling parameter, which helps direct the movement of particles in the air. If a particle cloud is generated in a construction zone, it should remain there with pressure control. Airflow control can be enhanced by using a window fan to pull air from inside the building to the outside. Careful control of an air supply to an exhaust fan ensures consistent negative pressure in a construction zone. The factors for such pressure management require a sufficient offset of supply-air vs. exhaust/return-air volumes. The amount of leakage in a special-ventilation (SPV) room or area is an important factor in providing consistent airflow management. The CDC's "Guidelines for Environmental Infection Control in Health-Care Facilities" describes a leakage of 0.5 sq ft per room. Some builders describe leakage in square inches per 100 sq ft of surface in a room. Studies that have seen leakage from 5 to 25 sq in. per 100 sq ft in AII rooms have been conducted. This leakage-area standard for SPV areas in hospitals has not been addressed, other than "sealing the rooms." The respective SPV rooms should be tested by pressurizing each room prior to occupancy. Leak areas in rooms can be found using maximum air volume offset and a smoke generator to find the leaks. When air streams out of a room through a leak, the air stream is seen, and the leak is sealed with caulk.
An important risk eliminator is to validate functional parameters of a room. Air exchanges need verification using an air-balance hood. Pressure monitoring can be conducted with a hand-held micromanometer (such a device should be sensitive to 0.0004 in. wg, or 0.1 Pascal).
Tools of the Trade
Smoke sticks, while useful, only provide qualitative information to ensure proper airflow direction. A smoke stick does not determine pressure.
Pressure gauges can be mounted on a wall in SPV rooms (AII or PE). Also, pressure readings can be taken with hand-held pressure monitors. The monitors should be checked often for calibration. One method is to verify that a wall-mounted monitor reads zero when the room door is open.
Particle counters are useful to ensure appropriate filtration. Often, the air quality in health-care facilities is monitored for microbial content. However, such monitoring is time-consuming for culture results. Therefore, a particle counter can be used for surrogate air-quality analysis. The interpretation should be based on air particles greater than 0.5 m in diameter. The data should demonstrate a rank order: The cleanest area with the lowest counts should be in the rooms with the best ventilation/filtration.
Volumetric air samplers should be used to measure particles in a given quantity of sampled air. In highly filtered environments, such as hospitals, large volumes of air must be sampled to find accurate culture concentrations. While culture methods are time consuming, microscopic identification of spore morphology is useful. However, qualitative analysis for Aspergillus fumigatus is not possible. Air sampling should verify air quality; rarely is it a predictor of disease because of the "snapshot" nature of the sampling process. It is better to work on validation of effective ventilation and control than air sampling to see what is present in an environment.
Summary
The validation of ventilation is best conducted before occupancy. The pressure gradient helps maintain the intensity of the airflow direction to contain or exclude hazardous/infectious particles from reaching a susceptible host. Pressure controls air movement, with airflow from high- to low-pressure zones. Pressure relationships control particles that ride on air currents. During construction and infectious-disease events, people must rely on pressure to help contain airborne contamination. Properly established and maintained AII and PE rooms should contain or exclude unwanted hazardous particles from reaching susceptible hosts.
Acknowledgement
The author wishes to acknowledge Andrew Geeslin for his technical assistance.
Bibliography
1) Sehulster, L., & Chinn, R.Y.W. (2003, June 6). Guidelines for environmental infection control in health-care facilities: Recommendations of the CDC and the Health-care Infection Control Practices Advisory Committee (HICPAC). Morbidity and Mortality Weekly Report, 52, 1-42.
2) Jensen, P.A., Lambert, L.A., Iademarco, M.F., & Ridzon, R. (2005, December 30). Guidelines for preventing the transmission of Mycobacterium tuberculosis in health-care settings, 2005. Morbidity and Mortality Weekly Report, 54, 1-141.
A registered environmental-health specialist, Andrew J. Streifel, MPH, has been helping hospitals worldwide resolve a host of environmental issues and establish safe patient-care environments for 30 years. He served on the revision task force for the 1996, 2001, and 2006 versions of the American Institute of Architects' "Guidelines for Design and Construction of Health-Care Facilities." He is a member of HPAC Engineering's Editorial Advisory Board.