Biosensors Aim to Detect, Attack IAQ Threats
Key Highlights
- The project focuses on real-time detection of airborne pathogens such as viruses, bacteria, and mold using biosensors similar to smoke alarms;
- Automated responses include increasing outdoor air intake, enhancing filtration, and activating germicidal UV lights to reduce bioaerosol concentrations;
- Initial testing will occur in daycare centers to address pathogen spread among children, with broader applications in schools, hospitals, and public spaces;
- The system aims to decrease respiratory illnesses by 25%, improving health, reducing missed workdays, and boosting overall quality of life;
- Funding from ARPA-H totals up to $40 million over five years, aiming to commercialize the technology for widespread use in various buildings.
By MELODY WARNICK, News Contributor, Virginia Tech
When a public building catches fire, its built-in systems automatically respond: Smoke alarms blare, sprinklers kick on, and occupants quickly evacuate.
But what if the life-threatening danger isn’t fire but invisible airborne contaminants that can make occupants sick? Could a similar smart-building system monitor and improve the quality of the air indoors, where Americans spend 90 percent of their time?
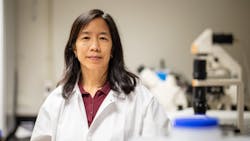
With a contract for up to $40 million from the Advanced Research Projects Agency for Health (ARPA-H), an ambitious multi-institutional research team led by Virginia Tech civil engineering faculty and University Distinguished Professor Linsey Marr, along with Senior Project Manager Aaron J. Prussin II, aims to create just such a system.
“The knowledge that comes out of this project will mean that when you go into a classroom, office, restaurant, or other building that has adopted the solutions from this research, the air is going to be cleaner and safer than it was before,” said Marr, who was recognized in 2023 as a MacArthur Fellow, also known as a 'genius grant,' for her research into air quality and the transmission of infectious bioaerosols. “That will mean that you have fewer days of illness, fewer missed workdays, and a better quality of life.”
The research
The research project, called Bioaerosol Risk Assessment interVention Engineering (BRAVE), has a goal of reducing respiratory illnesses, such as cold, flu, and asthma symptoms, by 25 percent with its own innovative clean-air version of a fire suppression system. Here’s how it works:
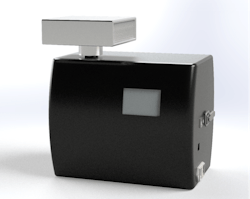
- A biosensor acts like a smoke alarm, using real-time detection of 25 viruses, bacteria, allergens, and fungi in the air, including SARS-CoV-2, influenza, respiratory syncytial virus, Legionella, and Stachybotrys chartarum, commonly known as black mold;
- Next, a suite of computational modeling software analyzes data from the building’s biosensors and other sources to assess risk for building occupants;
- When the risk is high, the sensor automatically communicates with the building’s HVAC system to amp up building ventilation with more outdoor air, increase filtration, or turn on germicidal UV lights in the ducts — interventions that have been proven to reduce concentrations of bioaerosols and reduce risk of illness;
- The system may even issue alerts and recommend behavior changes, like going outside or reducing building occupancy. But most of the time it will operate in the background, adjusting things as quietly as a thermostat.
The team will conduct the initial round of testing in daycare centers, where “there are lots of pathogens around, kids are getting sick, and their getting sick impacts parents and the whole community,” said Marr. “It's like a fire, and you want to put out the fire where it starts.” But what researchers learn there will be relevant in almost any communal setting, including classrooms, supermarkets, hospitals, and airports.
With the BRAVE approach implemented in these buildings, researchers expect that fewer children, parents, and workers will get sick, leading not only to higher levels of health and well-being, but to reduced absenteeism and improved productivity that makes clear that better indoor air quality is worth the investment.
“This $39.9 million award to Virginia Tech as part of the BREATHE program solidifies the university’s commitment to advancing indoor air quality solutions for the benefit of public health,” said Congressman Morgan Griffith.
The collaborators
As one of the world’s leading experts on airborne pathogen transmission, Marr will be the principal investigator of a large, seasoned, and highly interdisciplinary team, with subprojects led by Rajan Chakrabarty from Washington University in St. Louis (WashU); Madhav Marathe from the University of Virginia; and Chris Cappa from the University of California, Davis. Additional collaborators include:
- Amy Pruden, civil and environmental engineering, Virginia Tech
- Nisha Duggal, biomedical sciences, Virginia Tech
- Peter Vikesland, civil and environmental engineering, Virginia Tech
- Grant Brewer, Innovation and Partnerships, Virginia Tech
- John Cirrito, neurology, WashU
- Carla Yuede, neurology, WashU
- Meng Xu, energy, environmental & chemical engineering, WashU
- Michael Vahey, biomedical engineering, WashU
- Carolina Lopez, molecular biology, WashU
- Ron Kenyon, Biocomplexity Institute, University of Virginia
- Bryan Lewis, Biocomplexity Institute, University of Virginia
- Srinivasan Venkatramanan, Biocomplexity Institute, University of Virginia
- Baltazar Espinoza, Biocomplexity Institute, University of Virginia
- Aniruddha Adiga, Biocomplexity Institute, University of Virginia
- Parantapa Bhattacharya, Biocomplexity Institute, University of Virginia
- Przemyslaw J Porebski, Biocomplexity Institute, University of Virginia
- Dustin Machi, Biocomplexity Institute, University of Virginia
- Theresa Pistochini, civil and environmental engineering, UC Davis
- Rich Corsi, civil and environmental engineering, UC Davis
- Sarah Outcault, Energy and Efficiency Institute, UC Davis
- Jeffrey Hoch, health policy and management, UC Davis
- Emily Martin, epidemiology, University of Michigan
- Krista Wigginton, civil and environmental engineering, University of Michigan
- Khalil Chedid, epidemiology, University of Michigan
- Herek Clack, civil and environmental engineering, University of Michigan
- Jordan Peccia, civil and environmental engineering, Yale
- William Bahnfleth, architectural engineering, Penn State
- Gregory Pavlak, architectural engineering, Penn State
- Seema Lakdawala, microbiology, Emory University
- Johnson Controls
- Signature Science LLC
- Varro Life Sciences Inc.
“We’ve brought together an incredibly strong team of world-class experts in lots of different topics to focus on this one problem, because that's what we need to make a big leap forward,” said Marr. “There was a flurry of activity about indoor air inspired by the pandemic, and now we need to take the next step.”
The funding and the industry partners
ARPA-H is a government agency within the U.S. Department of Health and Human Services that supports the development of high-impact solutions to society’s most challenging health problems. Its Building Resilient Environments for Air and Total Health (BREATHE) program, through which the team’s contract is funded, focuses on smart building systems that monitor and respond to changes in indoor air quality as a way to revolutionize public health.
The initial round of funding is $20 million, with additional tranches to a total of $40 million over the next five years.
Ultimately, the team plans to commercialize its research so that the whole-building system, including biosensors, software, and engineering interventions, becomes a turnkey technology widely available for installation in buildings.
“Finding viruses in the air is like finding a needle in a haystack,” said Chakrabarty, the team lead from WashU in St. Louis. “It’s a grand challenge, but it’s exciting in the sense that here is an opportunity to really push the envelope of what is possible. Hopefully we can create a prevention mechanism to avert future pandemics.”