A New Hope for Building Occupant Health
Key Highlights
- Indoor air accounts for more than 80% of our daily exposure, affecting health, cognition, and immune function;
- Poor IAQ can cause inflammation, respiratory issues, chronic diseases, and impair cognitive performance, especially in vulnerable populations;
- Effective IAQ management requires continuous monitoring of pollutants, humidity, and outdoor air quality to inform ventilation and filtration strategies;
- Balancing ventilation with energy efficiency is crucial; demand-controlled systems and smart sensors enable optimal airflow based on real-time data;
- Microbiome-aware approaches promote microbial diversity by avoiding over-sterilization and incorporating natural materials, supporting immune health and building resilience.
by STEPHANIE TAYLOR, M.D., M. Architecture; ASHRAE Distinguished Lecturer; Medical Advisor, ThinkLite Air
Air is, by far, our most extensive exposure.
Every day, the average adult inhales about 13,000 liters of air, more volume than a week’s worth of food or water.i Moreover, the surface area of our tissues exposed to air (skin, upper airways, and alveoli in lungs) is equal to a full-sized tennis court! Spending over 80% of time indoors, the modern human has extensive and intimate contact with indoor air and all that it carries.
Despite the magnitude of this interface, we casually and often incorrectly assume that inhaled air is benign. We now know that managing indoor air quality (IAQ) properly is more than a matter of comfort or energy efficiency. It is a central determinant of health, cognitive performance, and the very survival of the human species.
IAQ and Human Physiology
Traditionally, IAQ management for occupants has focused on reducing odors and controlling sensible temperature for comfort. While comfort control is important, it is only the tip of the iceberg.
Every cell in our body depends on air for oxygen needed for survival, yet air is also the vector for potentially harmful chemical and microbial exposures. Primarily through breathing, and to a lesser degree through skin exposure, tiny particles, reactive gases, and volatile organic compounds (VOCs) enter our airways, with our bloodstream only a cell membrane away.
When inhaled air has low humidity such as during heating seasons, water from our respiratory membranes is extracted, desiccating our protective mucus membranes and impairing cilia movement – harming the first step of our immune defense. Within minutes, inflammation and oxidative stress can begin. Attention, productivity, and motor coordination measurably decline. Irritation of the nose, throat and sinuses results in coughing, tearing, and sneezing.
When lung airways are aggravated, they spasm - known as asthma or reactive-airway-disease. Longer exposure to even non-detectible contaminants contribute to chronic respiratory and heart disease, dementia, poor pregnancy outcomes and early death. In healthcare and senior living environments where occupants are often more vulnerable, poor IAQ correlates with higher rates of patient infections and staff absenteeism, along with use of more powerful antibiotics
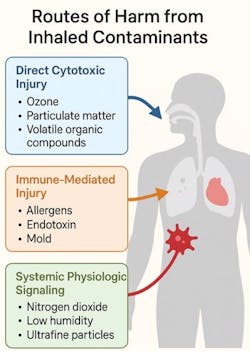
To summarize, poor IAQ affects the body via three routes:
1. Direct Toxic Effects – Reactive gases such as ozone, NO₂, and ultrafine particles penetrate deep into the lungs, damaging cells and disrupting genes.
2. Immune Dysregulation – Even low concentrations of pollutants trigger the immune system, stimulating inflammation that underlies asthma, cardiovascular disease, diabetes and neurodegenerative disease.
3. Systemic Signaling – airway irritation triggers stress pathways, influencing blood pressure, heart rate, mood, cognition, digestion, and increasing release of the immunosuppressant hormone, cortisol.
IAQ and Microbiomes
Recent advances in microbiology using genetic analysis tools have revealed dynamic communities of bacteria, viruses, and fungi, called microbiomes, that live within and on our body. Human microbiomes consisting of diverse microbial species help maintain almost every aspect of our physiological functioning, for example training our immune system to ward off invading and harmful pathogens, while dampening unnecessary allergic reactions.
Buildings, like humans, also host microbiomes that are shaped by outdoor air, materials, ventilation, and occupants themselves. Thus, IAQ management must not only reduce airborne contaminants, but also nurture a balanced indoor microbial ecosystem compatible with human health. (Figure 2)
Poor ventilation, excessively high or low humidity, or overuse of strong chemical disinfectants can drive the building microbiome through “survival-of-the fittest” to favor treatment-resistant, pathogenic species of viruses, bacteria, and fungal organisms. For example, low relative humidity (below 40%) increases airborne persistence of influenza and SARS-CoV-2 while drying occupant airways and harming protective mucosal surfaces that normally trap and neutralize microbes.
Similarly, excessive use of antimicrobial cleaners can remove beneficial environmental bacteria, allowing pathogenic (disease-causing) strains to dominate. IAQ management that ignores the indoor microbiome risks creating biologically hostile spaces.
Clearly, maintaining good IAQ is preventive medicine, not just mechanical maintenance.
How to manage IAQ for health...
1. Air quality monitoring
The first step in managing IAQ is knowing what indoor contaminants and humidity levels exist. Humans cannot perceive all important gases, particle levels and low humidity conditions that are harmful to health, therefore, questionnaires on comfort and satisfaction cannot provide these data points.
The only way to know what exists is to continuously monitor IAQ, and ideally surrounding outdoor air, with sensors that measure large to ultrafine particles, relevant gases, humidity and temperature. Trying to manage IAQ for healthy occupants and balanced microbiomes without this visibility is like driving on a dark road at night without headlights. You are asking for trouble! (Figure 3)
2. Ventilation and Air Exchange
Ventilating indoor spaces with outdoor air dilutes indoor pollutants – if outdoor air quality is good. Unfortunately, this is not always the case. Excessive ventilation with unconditioned or contaminated outdoor air can introduce pollutants such as ozone, carbon combustion by-products (e.g. nitrogen and sulfur dioxide, carbon monoxide) and increase energy consumption if extensive heating, cooling, humidification, or dehumidification are needed. Again, holistic and continuous indoor and outdoor air quality monitoring is necessary to effectively use mechanical demand-controlled ventilation, or even passive ventilation through operable windows.
3. Filtration and Purification
Mechanical filters in intake ducts or in-space units can effectively remove particles and allergens, while filters with activated carbon also capture VOCs and ozone. Bioinspired filtration using plant-microbe systems or enzymatic coatings represents an exciting next frontier, integrating natural detoxification pathways into engineered air systems.
4. Humidity and Temperature Control
Relative humidity between 40–60% is necessary for several reasons. This level of water vapor supports our mucosal defense, limits infectious bioaerosol transmission, and shapes microbial communities both within humans and within indoor spaces to favor diversity. To avoid condensation resulting in water accumulation and mold growth, proper insulation in building envelopes and cold surfaces must be maintained. Smart sensors and integrated controls can maintain proper ranges across climate zones and seasons.
5. Source Control
Preventing harmful off-gassing by choosing low-emission materials, managing cleaning products, and maintaining HVAC systems remains the most effective strategy. IAQ monitoring to detect sources, scheduled building commissioning, and following maintenance schedules are crucial.
6. IAQ Strategies for microbiome management
A “microbiome-aware” approach introduces ecological principles to IAQ management. Encourage Microbial Diversity: Avoid over-sterilization. Use cleaning products that remove soil but preserve microbial heterogeneity. Introduce materials like wood and natural fibers that host benign microbial communities and allow uptake and release of water vapor into indoor spaces to contribute to mid-range humidity that supports both human and microbiome health.ii
Health and Economic Outcomes
The benefits of healthy IAQ extend far beyond preventing discomfort or annoyance from odors. Improving IAQ reduces absenteeism, hospital-acquired infections, and cognitive fatigue. In offices, modest reductions in CO₂ and VOCs can improve decision-making performance by 8–11%.iii In hospitals, maintaining optimal humidity and filtration can lower respiratory infection rates by up to 30%.iv,v For building owners, these translate into measurable returns through reduced energy waste, liability, and healthcare costs.vi
Moreover, microbial stability itself can protect infrastructures: diverse surface microbiota inhibits fungal growth and biofilm formation that degrade materials. The convergence of health and maintenance benefits makes IAQ management one of the most cost-effective sustainability strategies available.
Ventilation and conditioning air account for 30–50% of total building energy use.vii The “traditional” response to IAQ concerns - increase ventilation—often conflicts with energy and carbon goals and can introduce harmful outdoor contaminants. New, affordable sensors and data integration allow “smart ventilation,” where airflow is determined by demand-controlled ventilation. Visibility into indoor and outdoor contaminant levels allow airflow adjustments based on pollutant loads rather than fixed schedules. These integrated strategies make “healthy efficiency” achievable—where energy conservation and air quality enhancement reinforce rather than oppose each other.
Our next step in IAQ management will hopefully merge technology with biology. Smart systems can learn occupancy rhythms and detect contaminant sources, adjusting remediation steps accordingly. Surface and duct coatings may incorporate living biofilms that metabolize VOCs, echoing how the liver detoxifies blood.
Materials may contain mycelium composites and bacterial cellulose which have pollutant-absorbing capacity. These bio-engineered solutions, imitating nature’s energy efficient, resilient, and self-regulating strategies are invaluable guides.
At the same time, occupant health monitoring via wearables or building-linked health dashboards can provide feedback loops. Correlating IAQ parameters with absenteeism, heart-rate variability, or cognitive performance will make the health impacts of air tangible and actionable.
Ultimately, IAQ management redefines the building as part of a larger living system. Our walls should not isolate and harm us. They should connect the occupants’ microbiomes, immune systems, and behaviors into a shared ecosystem. Healthy air can sustain both human and microbial diversity, while polluted or sterile air erodes resilience and fosters disease.
The challenge ahead is cultural as much as technical as we progress from viewing air as a mostly benign background to seeing it as a vital medium of health. Architects, engineers, clinicians, and facility managers must collaborate around this biological perspective. By doing so, buildings can become not just shelters, but truly a “New Hope” for improving human health.
####
Based in Stowe, VT, Stephanie Taylor, M.D., M. Architecture, is a medical advisor to ThinkLite Air; an InciteHealth Fellow at Harvard Medical School; an ASHRAE Distinguished Lecturer; and a member of the USGBC LEED Technical Advisory Indoor Environmental Quality Group.
References
i https://www.epa.gov/sites/default/files/2015-09/documents/efh-chapter 06.
ii Kembel, S., et al. (2012). Architectural design influences the diversity and structure of the built environment microbiome. ISME Journal 6:1469-1479
iii Allen, J. G., MacNaughton, P., Satish, U., Santanam, S., Vallarino, J., & Spengler, J. D. (2016). Associations of cognitive function scores with carbon dioxide, ventilation and volatile organic compound exposures in office workers: a controlled exposure study of green and conventional office environments. Environmental Health Perspectives, 124(6), 805-812. https://doi.org/10.1289/ehp.1510037.
iv Taylor, S. & Tasi, M.C. (2018). The Effects of Indoor-Air Relative Humidity on Health Outcomes and Cognitive Function in Residents in a Long-term Care Facility. ISIAQ Proceedings_Indoor Air, #744.
v Taylor, S. & Hugentobler, W. (2016). Is low indoor humidity a driver for healthcare-associated infections? “ISIAQ Proceedings _Indoor Air” Conference in Ghent, Belgium. https://www.condairgroup.com/humidity-health-wellbeing/scientific-studies/is-low-indoor-humidity-a-driver-for-healthcare-associated-infections
vi Shajahan, A., Waldram, J., & Wright, A. (2019). Effects of indoor environmental parameters related to indoor air quality in mechanically ventilated hospital buildings on patients’ healing and infection rates. Indoor Air, 29(3), 452-466. https://doi.org/10.1111/ina.12531
vii https://www.energy.gov/eere/buildings/heating-ventilation-air-conditioning-refrigeration-and-water-heating?utm_source=chatgpt.com